

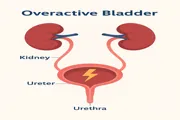
Overactive bladder is a syndrome in which an individual feels an urgent need to urinate, even without the presence of urinary incontinence. Is it a widespread condition? And where? It is a rather common condition—though not classified as a pathology—and is more prevalent in Western countries. Estimates suggest that about 8% of the population is affected, with peaks reaching up to 16%. The likelihood increases with age and clearly impacts quality of life.
Can it occur alone, or is it linked with other symptoms? It often coexists with frequent urination (known as pollakiuria) and nocturia, the need to urinate at night.
Does it affect men or women more? While both genders can be affected, it is more commonly observed in women. As for the causes, in many cases they remain unknown.
In other cases, overactivity may be linked to:
Are there specific contributing factors? Yes—the main one is age.
Age is a key factor, but not the only one. Other contributing factors include:
This syndrome can severely impact both physical and psychological well-being. It may affect relationships, sexual health, work, daily routines, and leisure activities.
Patients often develop anxiety due to fear of losing control over urination, especially at night, which may lead to poor sleep and even depression. The presence of incontinence may further amplify these psychological effects.
Recent studies show that quality of life in these patients is often worse than in those with other chronic conditions like:
Social discomfort is common. Many patients experience persistent unease, which can affect their ability to maintain relationships and participate in everyday social contexts.
Diagnosis typically starts with a specialist consultation. The patient describes symptoms like urgency, frequency, or nocturia. The doctor may recommend urodynamic tests to assess involuntary bladder contractions, the primary cause of overactivity.
These tests can be invasive and are only used if necessary—especially if obstruction of the urethra or bladder neck is suspected. Additional tests may include:
These are usually performed if infection is suspected.
Treatment may include lifestyle changes: avoiding caffeine and smoking, reducing liquid intake, maintaining healthy weight, increasing fiber, and regular exercise.
Pelvic floor physiotherapy can help control the urge by training pelvic muscles. Anticholinergic drugs may help reduce involuntary contractions, but they often cause side effects like:
These limitations highlight the need for new therapies.
People with this condition often experience a high level of social discomfort and perceive a persistent, generalized unease. This can significantly affect their interactions and daily relationships.
To diagnose an overactive bladder, a specialist will begin by collecting the patient's medical history and symptoms, such as urgency, frequent urination, and nocturia. In some cases, additional diagnostic procedures are used.
One common test is the urodynamic exam, which helps identify involuntary bladder contractions. This test is only performed when necessary due to its invasive nature. It becomes essential if there's a suspicion of an obstruction in the urethra or bladder neck.
Other possible tests include:
These tests are typically recommended if a urinary tract infection is suspected based on the symptoms.
There are several ways to treat overactive bladder. Lifestyle modifications are often the first step. Patients are advised to eliminate caffeine and smoking, reduce fluid intake, maintain a balanced weight, follow a fiber-rich diet, and stay physically active.
Pelvic floor physiotherapy is another effective approach. It involves exercises that strengthen the muscles responsible for bladder control. These techniques help reduce the urgency to urinate by modulating pelvic contractions.
Pharmacological treatment often includes anticholinergic medications, which are effective at reducing involuntary bladder activity. However, they are not always fully effective and may cause side effects such as:
Due to these limitations, ongoing research is seeking new and more effective treatment options.
It's also important to highlight that overactive bladder symptoms are often misunderstood or minimized by patients, which leads to a delay in diagnosis and treatment. Many people feel embarrassed to talk about urinary issues with their doctor, which contributes to underreporting and undertreatment of this condition.
The urgency to urinate may come suddenly and can be difficult to control, leading some individuals to limit their daily activities or avoid social events altogether. This self-imposed isolation can exacerbate feelings of loneliness and decrease overall mental well-being.
Healthcare professionals are increasingly recommending integrated treatment approaches that combine behavioral therapy, medical support, and patient education. Raising awareness about this syndrome helps break the stigma and improves health outcomes.
For more information, see the Wikipedia page on overactive bladder.
It’s a condition involving sudden, frequent urges to urinate, even without a full bladder. It may or may not include urinary incontinence.
Urgency, increased daytime frequency, nocturia (night urination), and in some cases, urine leakage.
Yes. It can lead to anxiety, social isolation, sleep disruption, and even depression in severe cases.
Behavioral changes, pelvic floor therapy, medications (e.g. anticholinergics), and experimental new treatments.
← Also read: Avoidance in Social Anxiety – causes and consequences